Weight loss
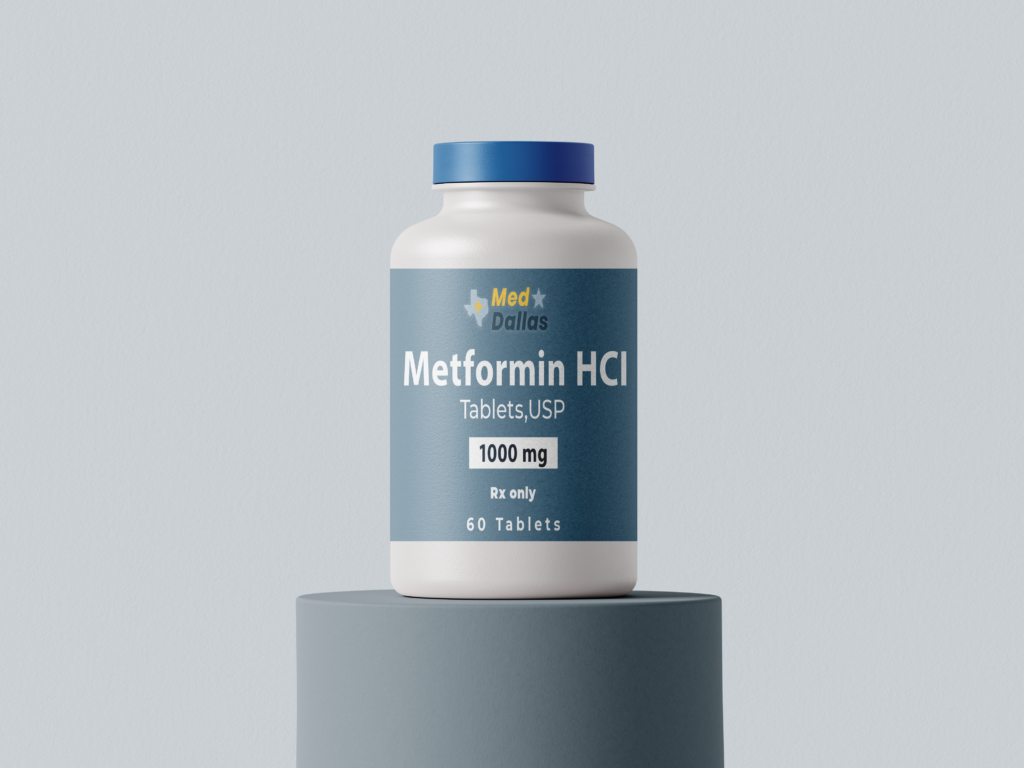
Metformin Tablets
Discover the benefits of Metformin Tablets, a trusted oral biguanide antidiabetic agent. Metformin is designed to effectively manage Type 2 Diabetes Mellitus and offers additional benefits for conditions like Polycystic Ovary Syndrome (PCOS). With options for both immediate and extended-release formulations, Metformin supports glycemic control, reduces insulin resistance, and provides cardiovascular protection. Learn how Metformin can enhance your health journey with insights into its usage, benefits, and safety considerations.
